I recently had a rare opportunity to perform an osteochondral allograft knee surgery.
A young, healthy female (18 year old) complaining of problems with her knee, presented with a severe defect which you can see in her MRI. This defect is in the weight bearing area of her knee, so continued pressure through the area was causing increased pain and swelling.
Treating large osteochondral (bone and cartilage) defects in the knee is complex, as simply replacing the defect with a prosthesis isn’t a feasible option in someone so young. Instead, opting for a biologic solution, with osteochondral allograft transplant can reduce pain and improve the function of the knee as well as potentially reduce the chances of her needing to convert to a knee replacement in the future. The fact that she is a young patient who doesn’t have arthritis or degenerative features, plays a big part in this decision.
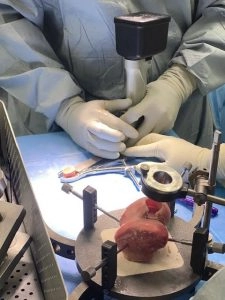
We matched the size and shape of the femoral condyle to a donor which was stored in a bone and tissue bank. I opt for fresh frozen storage as opposed to irradiated storage due to improved biological and biomechanical properties. We are fortunate enough to have access to a number of bone and soft tissue banks, which enables us to match the size and shape of the donor and recipient knees to optimise articular congruity of the joint.
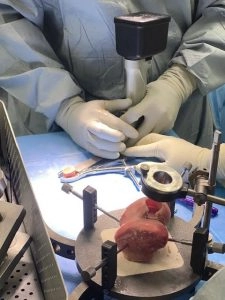
The osteochondral defect is sized at surgery, with resection of the damaged bone and cartilage and transplantation of a size and shape matched portion of cartilage and bone from the donor knee.
As an orthopaedic surgeon with an interest in the treatment of complex knee conditions, it’s been interesting to see the drive towards biological solutions to tissue defects. The surgery whilst complex, was very interesting and I look forward to following up the patients progress.
Stay tuned to find out more about the results of the surgery and the patient’s follow-up.
What is an Osteochondral Allograft
Osteochondral relates to bone and cartilage and an allograft is a tissue graft from a donor.
This means that in an osteochondral allograft surgery, donor tissue is used to repair damaged or lost bone and cartilage. The bone and cartilage which is transplanted, serve as a framework for the recipient’s own cells to indefinitely create new bone and cartilage.
Chances of the donated tissue being rejected
Tissue rejection is not a concern with bone and cartilage transplants and anti-rejection medication is not required for the patient.
The most common indicators for Osteochondral Allograft surgery:
- A 2 cm2 or larger localised cartilage lesion,
- Earlier cartilage surgery re-treatment,
- Re-treatment of microfracture, autologousosteochondral transfer, or autologous chondrocyte transplantation,
- Osteochondritis dissecans (type III or IV)
- Osteonecrosis (bone death)
- Reconstruction of a fractured joint
Osteochondral Allograft surgery follow up
It’s recommended that physiotherapy is started immediately after the surgery and a rehab protocol is followed. Patients who are undergoing large osteochondral allografts require a period of protected weight bearing, and a slow reintroduction to physical activity over a 3-6 month period. Depending on the complexity of the transplant, full recovery can take 6-12 months.
For more information about Osteochondral Allograft Knee Surgery or other enquiries, please visit our Contact page here.